If you are offering a group health plan to your employees, then you might need to offer continuation of health insurance coverage to certain employees and their beneficiaries. With COBRA coverage, qualified beneficiaries get the right to maintain group health benefits when they would be otherwise lost due to a qualifying event. Navigating through complicated requirements and compliance can be daunting for companies and employers. Kenz takes that burden away by offering COBRA Administration services, including documentation, compliance, payment collection, communication, etc. You can get everything done on our unified platform that provides all the information regarding enrollment, eligibility data, and benefits packages in the same place.
Our COBRA Administration solution offers you peace of mind by allowing eligible members quick access to insurance coverage that they are entitled to. They can select and pay for their coverage without worrying about the challenges of self-administered COBRA or file exchanges. Trust us for hassle-free COBRA solutions so you can focus on core business activities while we take care of compliance and accuracy.






 Download on the
Download on the
 Get it on
Get it on
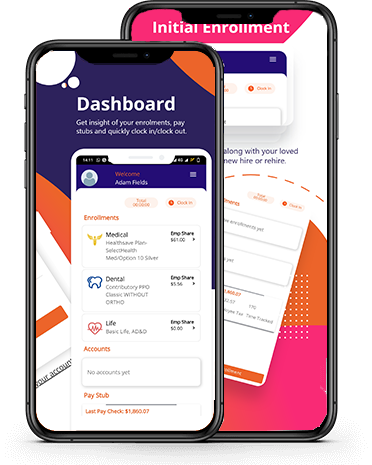



Kenz tracks the entire employee lifecycle, starting from enrollment to termination/resignation to COBRA administration. Each document and information is stored on a single record that you can easily view.