According to statistics, 15% of dependents covered under different health and benefits plans are ineligible for that coverage. This unverified enrollment costs millions of dollars to employers each year and is a major contributor to the rising costs of health insurance. Hence, employers must identify individuals who are not eligible and remove them instantly. So, how to verify the eligibility of dependents? This is where our dependent eligibility verification services come to your aid. Kenz is designed to meticulously audit dependents, ensure compliance, minimize litigation risks, reduce stop-loss exposure, and save ample time and money for your company. Our automated eligibility audit solutions are easy to execute and integrate with other systems and you can instantly identify errors and forgotten forms.
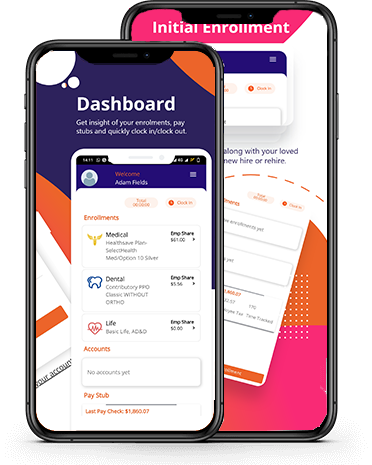
Run a one-time audit of entire employees and dependents and verify new ones continuously with our streamlined software. Integrated with the enrollment system, Kenz allows you to upload documents, review them, and get support whenever needed.










 Download on the
Download on the
 Get it on
Get it on